In January of 2008, I began having increasing difficulty with breathing. The problem was that I could not exhale as I used to. This caused hyperventilation. I had thought it was due to anxiety. I’ve had anxiety attacks in the past and this was quite similar. At one point, my then boyfriend (now husband) had suggested taking me to the emergency room of our local hospital. I declined. He asked why. I replied, “Because it might be cancer and I don’t want to hear that I have cancer.”
Of course, I did not know at the time how true my words were. My then boyfriend, now husband, Jerry suggested it would be better to find out if it is cancer because then I can fight it and be “okay.” I was afraid that if it was cancer, it would be the worst kind of cancer in the world and untreatable. This pattern of thought is tied into my PTSD issues. I assured him that the most likely reasonable cause is not cancer but anxiety and that I’ll be fine when the panic passes.
Another week or so went by and I began having more of these ‘anxiety’ attacks. Finally, one night, after several minutes of panting, I could not catch my breath and so Jerry called 911. The EMT coached my breathing to return to normal (like using a brown paper bag) because my oxygen level was 100%, I knew I was getting enough oxygen although it certainly didn’t feel like it.
The problem with exhaling was pain in my left side. Every time I blew out the breath I took in, a sharp stabbing pain would occur. The EMT and I both were convinced it was most likely caused by anxiety and that I would be okay. Jerry was not so convinced and insisted on my going to the hospital.
I had also developed a few other symptoms: drenching night sweats, extreme fatigue, a cough that was non-productive, and soreness under my left arm (in the armpit area). He felt it might be related. I thought it wasn’t as the doctors had already given me internal ultrasounds, cat scans and MRIs of my abdomen to try and determine the problem in the months prior to this incident. They never found anything.
They had thought perhaps I was entering into premature ovarian failure but blood tests ruled that out as well as ruling out cervical or ovarian cancer. In the months prior, I had this same sharp stabbing pain, but in my abdomen and not in my side.
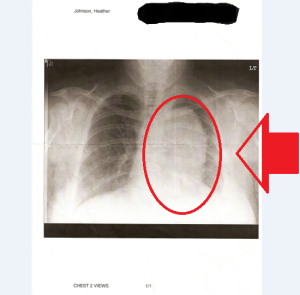
Well, so I went to the ER to let the doctors decide if it was all related. The doctor in the ER ordered a chest X-ray because he said my breathing was labored with some wheezing. The results of that showed a large white area on an X-ray. They redid the X-ray because the technician felt that she may have erred in performing the X-ray. The results again showed a large white area.
The doctor printed off a paper copy of the X-ray to show to me and with tears in his eyes he said, “This is your X-ray. That white area there,” he points to it, “is what I believe to be a tumor. You will need a biopsy right away to confirm this.” I just blinked at him. Continually. He asked, “You have children?” I replied, “Yes, 3.” At the time, I also had my niece in my home and I was her guardian. And, out of habit, I added: “They all have special needs.” He shook his head and the tears fell down his cheeks. I knew then that it had to be serious to make a doctor of his experience cry.
The report of the results of the X-ray states: “Again noted is the large mediastinal mass. There is a medium sized left pleural effusion associated with this process. The right lung appears clear. The trachea is midline. There is no pneumothorax. Conclusion: 1. Large mediastinal mass consistent with tumor. 2. Medium sized left pleural effusion.”
It is the pleural effusion that actually caused the difficulty breathing and pain, I think.
The doctor called for an ambulance transport to a Boston hospital called Brigham and Women’s Hospital. It’s a 45 minute drive from where I was living at the time. Jerry was at home with the children at this time as they could not be left alone. I called him from the ER’s phone and informed him of my impending ride to B&W’s hospital. I then called my father and asked him to go babysit the kids so that my husband could come up to the hospital to take the ride with me. Our local hospital is only five minutes away from our house; although it would have taken my father at least a half hour to get to the house. We had a neighbor whose daughter would have babysat until my father could get there.
But I didn’t like that plan all that much. I don’t like being visited in the hospital. I didn’t want my children to see me there either. What if something happened to me and that’s the last sight they see of me? No, I’d rather they have the last sight of me tucking them into bed. I don’t even like visiting others in the hospital. It’s part of my OCD issues.
So, I was to call from B&W’s with an update once I knew what was going to happen. The ER Doc from the local hospital sent me there with the intention that I would be admitted and have a biopsy right away. His thinking was that if it was a cancerous tumor, it was likely to be advanced and quick treatment would be my best chance at recovery.
However, upon arriving at B&W’s, I laid on the gurney in the corridor for a little while until an exam room became open. Then, once I was in there, I gave the ER attending physician my papers from the local hospital which included a CD copy of the X-rays. The doctor took it and came back several minutes later. She gave me a phone number and said to call that number in the morning and schedule my biopsy as no one is answering the phone at that time (they do not work late at night apparently). I said, “Okay.”And she walked away. A nurse came in and started the unplugging from various machines and I signed discharge papers. I called my father to come give me a ride home.
I was scared. The next morning, after the kids were off to school, I called the number the doctor in the E.R. gave me. I was told by the person who answered that “Patients cannot schedule themselves. You need to have the doctor call.” I explained what the doctor told me. She replied, “I don’t know who that doctor is but she should know better. I can’t schedule you.” and then hung up. I blinked for about an hour while staring at the phone wondering “Now what?”
I called my doctor’s office and spoke first to the receptionist, then to the nurse and then to the physician’s assistant. They told me not to worry and that they would get this handled for me. They pulled up the X-ray images at their office (they’re affiliated and can gain access through a shared network). They agreed with the original ER doctor who told me I needed to do a biopsy as soon as possible.
I was admitted to the Boston Medical Center in early February of 2008. I believe I “checked in” the night before the biopsy and left the day after. My father stayed at my house to help Jerry with the kids and making sure they got to school dressed in clothes that matched, had their lunches set, did their homework, etc. All the stuff I usually do. He even helped to clean up the place. As I mentioned above, I was experiencing some extreme fatigue and certain things had fallen behind. The place wasn’t very clean at all and it drove me nuts that I couldn’t… just COULD NOT clean it. I’d try too. And end up in pain, worn out and sleeping on the floor.
I was also given a CT Angiogram of the Chest with contrast test (A CAT scan of my chest with intravenous contrast) a couple of days later in prep for the biopsy. The conclusion from this scan was “Mediastinal mass and adenopathy most consistent with lymphoma. Increase in size of left pleural effusion.” This explained why the pain was getting worse in my side when I tried to breathe.
I also underwent a PET scan for staging information. The PET scan went from the base of my skull to the thighs. The conclusion of this stated: “There is intense activity associated with enlarged anterior/superior mediastinal mass and enlarged lymph nodes in the right paratracheal region, subcarinal region, and left infrahilar region abutting the pericardium. The imaging appearance is nonspecific but I would consider lymphoma the most likely possibility for this imaging picture. Alternatively, this could represent metastatic lymphadenopathy. Tissue diagnosis is warranted.”
I got the results of the biopsy on February 22, 2008, when I had my first oncology appointment with Dr. White (no relation). She asked if I knew anything about the type of cancer I have. I said I didn’t as I have not yet been informed of the results of the biopsy but that since my doctor’s office scheduled the appointment with an oncologist, I had assumed that meant the mass in my chest was, in fact, cancerous. She confirmed this.
She stated to me that I have Non-Hodgkin’s Lymphoma. She said the technical term for the particular type of Non-Hodgkin’s Lymphoma is “Stage IBX grade III follicular lymphoma with bulky mediastinal adenopathy”. I recall her telling me that if I had to get cancer, this is the best type of cancer to have because it is easily treatable. She told me that I would undergo 6 rounds of out-patient chemotherapy (the type of chemotherapy I received was called R-CHOP) and follow with radiation treatment, probably 27 treatments.
At another appointment, Dr. White attempted to do a bone biopsy to determine whether or not the lymphoma was in my bone marrow. They had given me a dose of Ativan (0.5 mg) to help calm me down. I had lain down on the exam table, on my stomach. She numbed the area and began poking around the site with her fingertips. This causes horrible amounts of pain. She was attempting to get this bone biopsy from around my hip bones. With the degenerative joint disease and fibromyalgia, using her fingers to poke around my bones was quite painful. The doctor decided to have me do the bone biopsy the next day under conscious sedation. It went much smoother as I fell asleep while they were doing it and didn’t feel a thing. The results of the bone biopsy showed that the lymphoma was not in my bone marrow. This was very good news.
I began chemotherapy on March 5th, 2008. I went, accompanied by Jerry. It wasn’t as bad as I thought it would be. There were several chairs around the room (curtains for privacy if one wished for it) and individual TVs. They also fed us lunch while we were there. Because of this, to this day, when I try to eat in a hospital cafeteria, I get sick to my stomach. It’s all psychologically related to me now. The first day after the treatment, I felt good. The second day? Not so much. I had trouble stopping the nausea and vomiting even with several prescriptions that were supposed to do that. I would take a pill and it would come back up. The third day was even worse. I discovered that I no longer could drink my favorite coffee (from Dunkin’ Donuts). My tastes had changed and coffee no longer appealed to me. Over all though, the first week wasn’t too bad if I could remember to take my anti-puke pills on time (before the previous one actually wore off).
The second week was difficult. I could not seem to get out of bed and often had to use a urinal by the bed. I kept myself occupied with a laptop and many books. Because I was so weak and tired, I had the kids start joining me in my room to watch TV with me. My niece and I would watch “America’s Next Top Model” while doing each other’s hair or nails. Once I even used Sharpie markers to draw a “tattoo” on her back of her name. Bboy would just sit in my room as he wasn’t as talkative then. Thomas would fill in the silence and tell me about every minute detail of his day at school and after-school program. I treasured those moments. I felt that I was able to still interact with my family.
The third week I was still experiencing nausea and vomiting. I ended up in the E.R. for treatment to stop the vomiting and for dehydration. I was still weak and still oh so tired. It seemed I could only drink Mountain Dew and eat Ramen noodles, chicken flavored, in order to not get sick. But I did feel better towards the end of the third week.
When I went in on March 26, 2008, I told them that I did not get better during the second week as I was told to expect to and that the nausea and vomiting did not stop after the first week as I was also told would most likely happen. The doctor explained that because I was so young and still menstruating, that chemotherapy will be harder on me. She explained that this disease usually only occurs in those who are 60 years and older. Because of my age, she said, I may experience more difficulty and the “recovery” time between treatments may not work out the way they usually do for older patients.
The second time around was not as bad as the first time. I think this is because I knew more of what to expect and so the shock of the reality of the side effects of chemo had worn off and didn’t seem as bad. Plus, I was learning what would bother my stomach now.
However, on Easter of that year, as I was beginning preparations for cooking Easter dinner, I noticed long strands of hair falling out. I was losing my hair again. I asked hubby to give me a hair cut with the razors. He hated to as he loved my long hair as much as I did. But well, I wanted to eat my Easter dinner without the risk of also eating my hair! So, he gave me a buzz cut. Within the next two weeks, the stubs had fallen out and I was totally bald… within a month, I had no hair on my body anywhere. I was relieved to not have to shave my legs to get that smooth silky feeling!
My third round happened on April 16, 2008. This time around I didn’t do too badly at all. I did develop a sensation on the bottoms of my feet that felt like I was walking on pins and needles. The doctor decreased the amount of one of the drugs in the R-CHOP chemotherapy drug cocktail that I was receiving. She stated this should lessen the frequency/intensity of the neuropathy in my feet.
My fourth round of chemotherapy occurred on May, 7th 2008. The nauseas was still present as ever but during this round, there was no vomiting. My breathing had improved. My cough had gone away completely. I was feeling in good spirits even though I was still feeling extremely tired and having difficulty sleeping.
My fifth round of chemotherapy occurred on May 28th 2008. This round found me tired and in pain as my fibromyalgia had flared up and was causing extreme pain and lack of sleep. But other than that, I had tolerated this round of chemotherapy quite well in my opinion.
I received my sixth and last round of chemotherapy on June 18, 2008. I was relieved it was going to be the last. I had felt better in the days leading up to this latest rounds and several imaging tests along the way showed that the mass had shrunk so I knew the chemotherapy was working.
During the meeting with the medical oncologist, I informed them that I would be moving because my landlord would not allow Jerry to sign on to the lease. The landlord does not like allowing males as tenets, as it appears from the people that lived in the low-income housing area where I was residing at the time. All legal tenets were females, some with children and some without. None of the men living in these units were officially on the lease. The women had told me that they had tried to put them on the lease and all their requests were denied.
Instead of fighting with the management company over this, I decided to move to Oklahoma where Jerry was still paying rent on a house. It’s more cost-effective living in Oklahoma as the prices for rent are much lower than what I could get in MA. I was not going to have Jerry live with me illegally. That would be wrong.
The doctor asked me if there was a way that I could afford to stay living nearby (as in move into a hotel for a few weeks) as the radiation treatments are done daily and would be finished most likely within a month. Jerry and I pursued that option but we could not, at that time, afford an extended-stay at a hotel.
Since we couldn’t, the doctor’s office tried to locate several radiologist oncologists in Oklahoma but none of their searches turned up any. Jerry suggested to them to try Ft. Smith as it is close by and accepts the Medicaid insurance from Oklahoma as well as Arkansas. I was given a piece of paper with a doctor’s name and phone number and address in Ft. Smith. I was told that this was a general practioner in Oklahoma and that I should make an appointment with her as soon as we arrived in Oklahoma and that this doctor would provide the necessary referrals to a radiologist oncologist to begin my radiation treatment. The activities described in this paragraph took place over the month of July in 2008.
I was told then that a month off between chemotherapy and radiation would not be a huge deal as the last PET scan came back “clean enough.” BUT Dr. White told me that I *must* see a radiologist as soon as possible once I arrive in Oklahoma. I quite clearly remember her vehemence on this matter. I assured her I would do so.
We arrived in Oklahoma on August 8, 2008. We drove over 1800 miles, with two special needs boys, two birds and one cat, hauling a small U-haul trailer on the back of our van. We ended up having to stay in a hotel for the weekend because the house was not move-in ready. From the hotel, I scheduled my first appointment with the doctor in Ft. Smith. It turns out that she is only a “fill-in” doctor at the hospital’s clinic for urgent care. Urgent care is care that is needed urgently but not an emergency. However, she referred me to another doctor affiliated with that hospital and I made an appointment with her. My husband made his first appointment with this doctor’s husband. They shared the practice.
At my first appointment in August, I asked for a referral to a radiologist oncologist. The doctor told me that she was new to the area and didn’t know anyone offhand. She stated she would have “one of the girls” look it up for her and call me when they get an appointment for me. I scheduled my next appointment with her for the following month. I did not receive a call from her office during that time letting me know my referral had been given and/or an appointment.
So, in September, I saw this doctor again. And again, I request a referral to a radiologist oncologist for radiation therapy. She asks me why do I want to see a radiologist oncologist. After picking my jaw up off the floor, I responded with, “Because I have Non-Hodgkin’s and my medical oncologist back home stated very clearly that I need to do radiation therapy to finish the treatment protocols.” She nodded and again said she didn’t know of any in that area. I said, well, do you have a phone book? Maybe I can look it up?
Her assistant brought in a phone book but there were no radiologist or medical oncologists listed in the phone book. I swear I have never seen a phone book not advertise doctors by specialty before. I suggested she ask a colleague at the hospital if they would know one. I said it didn’t even have to be in this area. I was willing to travel to finish my treatment.
Another month went by. And another. And another…. Finally, the doctor tells me she has received my medical records from the oncologist in Massachusetts and that my last PET scan was “negative” for cancer-like activity. I said “Yes, I was told that it was “clean.”.” She nodded and said, “Okay, so what would the radiologist radiate?” I kind of looked at her funny. She further said, “Well, if there’s nothing there, there’s nothing to radiate. You’re cancer free. Why go for treatments that aren’t necessary?”
I admit… I loved hearing those words. Looking back in hindsight, I can see where I should have been more skeptical of what this doctor was telling me and I did mention to her at that time that it didn’t sound right because my medical oncologist was so insistent about it. This doctor replied, “Well, since the PET scan results are the last in the medical records, maybe she didn’t get them before she told you that.” That made sense to me. Maybe it made sense to me because I *wanted* it to be over. So, I let it go.
My husband began having more difficulty in breathing at about this time. His doctor ordered a sleep study. It took them almost 2 months to get it scheduled. Then it took them another month to get the results back. Because this office kept dilly-dallying around with getting things done, the next time I went to the ER, I went to our local one and asked the ER Doctor for a name of a local doctor who could be my new GP. I got lucky that he was taking new patients.
We’re now into the summer of 2009. I gave my new doctor the history of the past year or so. He was rather shocked at what I told him that the doctor told him. But what I had said was confirmed in the doctor’s notes from those visits, “Patient requests referral to a radiologist oncologist.” and then shows no one made any calls or follow-up. The doctors at that practice blamed the staff supporting them. The doctors said that they could not hire and fire their own staff as the practice actually belongs to the hospital (it is on hospital grounds). My new doctor got me a referral and an appointment with a radiologist oncologist in Ft. Smith. It was about two miles away from the old doctor’s hospital. Sweet, huh?
I went to my first appointment (consultation) and was told that the first GP I had was wrong about not needing radiation. She told me that while a PET scan may come up “clean” after chemotherapy, radiation is still necessary as the cancer cells may be as small as to not show up. I was upset with myself at this point. I should have insisted on the referral and/or found another doctor sooner. Bells had gone off in my head and I failed to listen to them because I *wanted* what she told me to be true.
I was reassured by the radiologist oncologist (RO) that it was okay. I could begin radiation treatments right away. They scheduled me for 28 treatments. I was to go Monday through Friday, every day, twenty-eight times. There is an hour’s drive there and back.
I did end up getting sick from the radiation in a way. I got severe sore throats, would lose my voice at random, I developed a cough that was non-productive, I began getting night sweats again. And I was tired again. I was told that all these symptoms were side effects of the radiation. I did miss a few of the treatments because I was just too tired and could not even get out of bed. At one point, the doctor ordered a break because I had caught a cold and was doing so horribly with the treatments. I had taken a week off and then had to begin again.
I was told sometime later that I had a mass in my chest. They did not know whether it was scar tissue or cancer. They felt it was most likely scar tissue. They stopped treatments (saying that radiation in some patients may cause cancer growth?!?). Apparently, they had known about this mass since my first CT scan they did in preparation for the radiation treatment. I began receiving CT scans about every other month or so. Just to “wait and see” what develops.
Finally, in April of 2010, I demanded a PET scan. The doctor that saw me that day was the physician’s assistant to the RO. She said “You can have PET scans, can you?” and starting rummaging through my medical record. Then she said, “Oh, you’ve had one before. I must’ve had you confused with another patient.” Which makes me think they’ve had me confused this whole time and that is why they’d been only doing CT scans. Grrr..
The PA said that she would have to ask the RO to sign off on the PET request and my referral request to a medical oncologist (to discuss further treatment options). I stopped at the front desk to wait for them to get me an appointment with this RO as a follow-up. They said they’d have to call me with an appointment because they wanted to make sure it was after the PET scan and that the report from that PET scan would be back in. So I went home.
From 2 days after that appointment to several weeks later, I began calling their office almost daily. Those that know me, know what a chore that is for me. They kept insisting they needed the RO’s okay on it and that they would call me. Again and again I was told that.
Finally, I told my new GP what was up. He called and confirmed with that office what I had told him (that I was *still* waiting on my PET scan appointment and referral to a medical oncologist). He confirmed it and then said he’d get it done for me. Which he did. Well, actually his nurse set up the appointments but on his orders. I love his nurse!
At the end of July, I received a post card that was mailed on July 28, 2010 informing me that I had missed my appointment with the RO of July 29th, 2010. Amazing how they knew I was going to miss my appointment with their office a day ahead of time, huh?
Now here it is, the end of September. I’m happy to report that treatment was successful. The mass in my chest that 10 cm in April has shrunk to less than 1 cm and is “dead” according to the latest PET scan.
At my last oncologist appointment, after giving me the good news, I was told that I would need to be monitored fairly often (my next appointment with him is in four months) because with the type of lymphoma I had, it is likely to come back again within the first two years. While I most likely won’t get the same type of lymphoma again, I will likely get another kind. But that those types of cancer do not normally require aggressive chemotherapy and I’m not likely to lose my hair… AGAIN.
To celebrate this, I dyed my hair back to its “original” color. You see, after losing your hair several times, it tends to grow back in darker. It also grew back in once curly. It’s straight again now though but was considerably darker and I had no red hair at all left. I loved being a red head. So, Thank you Clairol!
Thank you to my family for their support during this time. Thank you to all who prayed for me. It worked! Thank you to my friends who have supported me.
I have won this latest battle and will continue to fight to stay healthy. I remember my mother’s mom having cancer on and off for 20 years. She started out with the same type of lymphoma I had started with. Knowing that she lived a long life anyway, gives me hope that I can do the same!
[EDIT: In September of 2013, I went to an oncology appointment with a new oncologist, Dr. Sjak-Shie. She is affiliated with Mercy Hospital in Fort Smith, Ar. She studied in L.A., CA and other areas. She told me at that appointment that I would *always* have the follicular lymphoma and that it never really goes away. It becomes so miniscule that you cannot see it on any scan but blood work will show the inflammation and infection such as when one has this cancer. She said that it will stay dormant for a period of time and that then it will flare up again. Patients like me will have to decide on when to treat. The problem with treating every time is that R-CHOP therapy (the best course of treatment in her and many oncologists’ opinions) is hard on the body, particularly between the ages of adolescence and 55. Basically, if you’re a woman who menstruates still, it’s going to suck worse for you. So, over time, R-CHOP damages the body just as bad if not worse than the cancer so they usually wait to treat until the cancer has caused “life-threatening” side effects. I may have symptoms (and I do now) but it does not always necessitate treatment at that point. So, I have not had any treatments in 2012, 2013 and none so far in 2014). ]
3/27/14
Information on the prevention of breast, colon, lung, and prostate cancers is not provided in this article. Children School Books
You’re correct in that information on the prevention of breast, colon, lung, and prostate cancers is not provided in this article. For one, I did not have breast, colon, lung and/or prostate cancer. For two, this is my personal account of my life and treatment of Non-Hodgkin’s Lymphoma and was not meant as a medical information article.
I would suggest readers looking for that type of information go to a website such at that by the Mayo Clinic, http://www.mayoclinic.org or use a search engine with those as keywords to find sites with that information.
Reading this was like reliving those days for me. Remember the “attitude” we got from the guy admitting you the night before your biopsy? I think I was ready to smack him. He even had his coat on so he could leave after dropping us off at the floor where you were to spend the night…
I love you, Heather. You’re my fighter and I’ll stand by you always…
Jerry
I had forgotten all about that! The sitting in his dark office while he ignored us cause he wanted to go home and he had to check us in first. I remember that now! Wow.. yeah.. it was fun walking down “memory lane” so to speak.
Heather, you are such a fighter and that is why I love you. I wish you the best in life because you deserve it so much.
Thank you, Tina! Thank you very much for the sweet words 🙂
What’s Happening i’m new to this, I stumbled upon this I
have found It absolutely helpful and it has aided me out
loads. I am hoping to give a contribution & aid different users like its aided me.
Good job.
Brachytherapy could also be recommended by oncologists along with external beam therapy.
The advance stage of breast cancer is observed to be the highest among the Malay ethnic group.
A positive attitude is essential to being able
to fight cancer, so you should never give up.
Hi to every body, it’s my first visit of this weblog; this blog contains awesome and genuinely excellent stuff designed for
readers.
There is definately a lot to learn about this subject.
I really like all of the points you made.
You’re so interesting! I don’t believe I have read through something like that before.
So nice to discover someone with a few genuine thoughts on this subject matter.
Seriously.. many thanks for starting this up.
This web site is something that is needed on the internet, someone
with some originality!
Well, thank you!
You ought to be a part of a contest for one of the highest quality
blogs on the web. I am going to highly recommend this website!
A fascinating discussion is definitely worth comment. I believe that you
ought to write more on this topic, it might not be a taboo matter but
generally folks don’t speak about these subjects. To the next!
Best wishes!!
Hi, always i used to check blog posts here early
in the dawn, as i love to gain knowledge of more and more.